
By Emma,
Honestly, a few years ago I didn’t care much about diabetes. That all changed the day my dad told me he’d been diagnosed with Type 2 diabetes. Since then, I’ve been his ‘guinea pig’ of sorts helping him find ways to lower blood sugar.
I’d usually test things on myself and my husband first. If that worked, then dad gets to try. We found it was safer this way since dad’s glucose levels can really jump up significantly with the wrong foods.
The thing is, my dad’s the type who likes eating buffets. His favorite food is a big slab of ribeye steak with mashed potatoes. And, besides his golfing, he hates exercise. In fact, he’ll always try to find the nearest parking slot to where we’re going. And, gets frustrated if he doesn’t since he has to walk an extra 20 meters.
So the goal was to find simple ways that he’d agree to follow consistently. Thankfully, we did. Now, his Hemoglobin A1c (HbA1c) stays in the 6’s. But, he does still have days when he goes off track. And when that happens, his morning blood sugar shoot up the next day.
Here’s a list of the things that I’ve found over the past 3 or so years. As you can see, I’ve spent a lot of time researching. But, that’s what you do after hearing all the things the doctor had to say about what could happen if dad didn’t get his blood sugar under control.
Like dad, try to find the things that you can incorporate easily into your diet and lifestyle. We’ve found that’s the best way to stay consistent. Do take a special look at the post meal section, that made a huge difference for my pops.
Overview of Type 2 Diabetes
As of 2015, over 30 million Americans have diabetes. That’s close to 10% of the population. Additionally, another 84 million individuals were pre-diabetic, which is a pre-cursor to type 2 diabetes.
Diabetes happens when your body isn’t able to produce enough insulin to clear glucose from your blood. As a result, you experience high blood sugar.
For anyone trying to control your numbers or avoid diabetes, here are 60 simple ways to lower blood sugar naturally. Combine a few of the different methods below to improve your health and overall well-being.
Table of Contents
- Lifestyle Choices and Changes
- How to Lower Your Blood Sugar Naturally with Diet
- Bring Down Your Post Meal Blood Sugar Fast
- Vitamins, Minerals, Herbs, and Supplements for Glucose Control
- Diets for Blood Sugar Control and Reduction
How to Lower Blood Sugar without Medication
Lifestyle Choices and Changes for Lower Blood Sugar
1. Lose Some Weight
 Excess body fat and a high body mass index (BMI) are the highest indicators of diabetes risk. Also, a larger waist circumference is linked to increased risk.
Excess body fat and a high body mass index (BMI) are the highest indicators of diabetes risk. Also, a larger waist circumference is linked to increased risk.
Additionally, studies note the importance of body fat distribution. Your waistline is an indicator of how much abdominal fat you have. And, the larger your waistline, the higher your risk.
Studies indicate that waist circumferences that are greater than 40 inches (for men) and 35 inches (for women) up your risk of high blood sugar, insulin resistance, and risk type 2 diabetes.
More importantly, weight loss from calorie restriction and exerci se help reduce the incidence of diabetes by 58%.
Bottom line is, maintaining a healthy weight and keeping your waistline in check is important in preventing high blood sugar.
2. Fix Your Diet Composition
In addition to calorie restriction, another powerful tool to help you lose weight is diet composition. Research states that improving the makeup of your diet reduces the incidence of diabetes by up to 87%
It notes 3 main issues with diet composition associated with type 2 diabetes. These are:
- Low fiber intake
- High trans fat and low unsaturated fat consumption
- Absence of or excess alcohol
It also estimates that over 90% of the general population have at least one of these risk factors. Thus, fixing these issues will help you lower your risk of high blood sugar and diabetes.
For those who have a hard time losing weight, adjusting your diet’s composition may be the answer. A 2006 study shows you can control blood sugar in type 2 diabetics without weight loss.
Here, the researchers increased protein in the diet from 15% to 30%. To compensate for this, they brought down the number of carbohydrates for each meal from 55% to 40%. They kept fat content steady at 30%.
 The chart above shows the lower blood glucose excursions after each meal due to the higher proportion of protein.
The chart above shows the lower blood glucose excursions after each meal due to the higher proportion of protein.
The study also discovered that adjusting fat content makes a difference.
Modifying the diet to one with 30% protein, 20% carbs and 50% fat reduced 24-hour glucose by 38%. This brought the fasting blood sugar levels of the diabetic subjects to near normal. A 30% protein, 30% carb and 40% fat diet also produced similar results.
3. Make Exercise a Daily Habit
 Exercise is something everyone should do. The human body is designed to move. Unfortunately, the digital age has made this more difficult.
Exercise is something everyone should do. The human body is designed to move. Unfortunately, the digital age has made this more difficult.
Physical activity of any kind helps the body use up glucose.
You can walk, clean the house, do some gardening or hit the gym.
This prevents it from accumulating in your bloodstream causing high blood sugar. Additionally, exercise helps you lose weight. It also aids in improving cholesterol and blood pressure levels.
Danish researchers note that the 80 to 95% risk increase of diabetes caused by obesity can be mitigated by physical activity. They recommend a Physical Activity Level (PAL) value of at least 1.8, which is being moderately active. This PAL level amounts to around an hour a day of physical activity or exercise, like the weight lifting or jogging.
Type of Exercise, Duration and Intensity and Their Effects on Blood Sugar
So what exercise is the best for blood sugar? How long should it be done? And, how much intensity do you need?
Data from the Big Blue Test offers some answers. The Big Blue Test is an annual initiative by the Diabetes Hands Foundation. Here, diabetics voluntarily record their levels of physical activity. And, the resulting blood sugar readings.
These are the relevant figures gathered from the 2012 Big Blue Test.
Most Popular Types of Exercise
Walking was by far the most popular form of exercise. Its simplicity makes it easier for anyone to do.
 Walking: 48.5%
Walking: 48.5%- Other types of exercise: 18.7%
- Running or Jogging: 11.9%
- Cycling: 8.8%
- Conditioning machines: 6.4%
- Dancing: 5.7%
Engaging in exercise reduced mean blood glucose levels by 31.3 mg/dL (-16.8%).
But, it’s worth noting that exercise was only effective 76% of the time. Blood sugar was unchanged 9% of the time. And, in the remaining 15% it increased.
Unfortunately, the data doesn’t mention why. But, the level of intensity and duration may be factors.
Which Type of Exercise is Most Effective for Blood Sugar?
While walking was the most popular, it produced the least reduction. On the other hand, cycling and running offered the best results.
In general, the more physical activity involved the larger the decrease in post-meal blood sugar levels.
- Cycling: -42.4 mg/dL
- Running or Jogging: -40 mg/dL
- Dancing: -37.4 mg/dL
- Conditioning machines: -35.9 mg/dL
- Non-specified exercise: -33.45 mg/dL
- Walking: -25 mg/dL

Exercise Intensity
Interestingly, high intensity exercise resulted in a smaller decrease in blood glucose. This tells us that moderate intensity is optimal.
- Vigorous exercise: -28 mg/dL
- Moderate exercise: -32.7 md/dL
Duration: How Long Should You Exercise?
When it comes to how long you should exercise, it’s simple. The longer the better.

The chart above shows a general downward trend as the duration of exercise got longer.
Reduction in Blood Sugar Based on Duration of Exercise (in mg/dL)
| All Exercise | Moderate Intensity | Vigorous | |
| <=10 min. | -17.9 | -16.9 | -25.1 |
| 11-19 min. | -25 | -25.6 | -22.1 |
| 20-29 min. | -30.9 | -29.9 | -36.1 |
| >=30 min. | -34.5 | -39 | -27.6 |
How Long Do You Wait After Eating?
On average, exercising 1 or 2 hours after eating produced the best results. The two showed similar 40.1 mg/dL reductions in blood glucose.
Meanwhile, engaging in physical activity 30 minutes after eating saw a decline of 28.6mg/dL. Doing so after more than 3 hours post-meal produces a 21.2 mg/dL drop.
What’s the Best Combination?
The largest blood sugar decrease was seen with exercise done for more than 30 minutes 1 and 2 hours after eating. The reductions were -49.3 mg/dL and -46.4 mg/dL, respectively.
In contrast, the same exercise duration done 30 minutes after eating produced a 34.3 mg/dL improvement. And, one after 3 hours helped by 19.6 mg/dL.
For those who don’t like regimented physical activity, you can do chores like vacuuming, or partake in hobbies like gardening.
4. Do Less Sitting
 In contrast to being active, sitting down for long periods should be avoided. A sedentary lifestyle increases post-meal blood sugar and triglyceride excursions. It also harms insulin sensitivity.
In contrast to being active, sitting down for long periods should be avoided. A sedentary lifestyle increases post-meal blood sugar and triglyceride excursions. It also harms insulin sensitivity.
Research reveals an inverse relationship between time spent doing low-intensity physical activity and blood sugar. Specifically, the more physically active you are, the lower your 2-hour Glucose Tolerance Test (GTT) levels are. This includes low intensity activity as shown in chart A to the right.
Meanwhile, the chart B shows the 2-hour Glucose Tolerance Test results based on the sedentary time.
As you’d expect, it’s the complete opposite. The more sedentary you are the higher the blood glucose gets.
What’s interesting is that just standing goes a long way.
- Alternating between 30 minutes of sitting and standing throughout the 8-hour workday lowers blood sugar levels by 11% on average.
- Similarly, a study reveals that standing 185 minutes after eating lunch reduces post-meal blood sugar by 43% compared to sitting down.
- Finally, research published in Diabetologia notes that sitting down after eating increases your risk of type 2 diabetes by 112%. This is over and above the 147% rise in cardiovascular risk. And, the 49% rise in other mortality risks including disease.
5. Drink Enough Water
Staying well hydrated helps keep your blood sugar at healthy levels. Water helps your kidneys flush out blood sugar. This is especially true when you’re hyperglycemic.
Drinking enough water also prevents dehydration. Dehydration increases your risk of high blood sugar. A study in Diabetes Care reveals that your level of water intake is inversely related to hyperglycemia. Because drinking water rehydrates you and lowers blood sugar, getting enough of it reduces your risk of diabetes.
The best thing about water is it doesn’t have any calories or sugar. As such, you can enjoy it without gaining any weight. Or, negatively affecting your blood sugar levels.
6. Manage Stress
 Stress wreaks havoc on your health. It also raises your blood sugar levels. This is because of the hormones your body secretes when stressed.
Stress wreaks havoc on your health. It also raises your blood sugar levels. This is because of the hormones your body secretes when stressed.
Stress causes your adrenal glands to increase production of hormones. These include adrenaline and cortisol. The stress hormones in turn, cause your liver to secrete glucose back into your bloodstream. This excess rush of glucose is what gives you extra energy. It also lets you focus better, have more strength, and be more alert alertness during emergencies.
With chronic stress, you’re in a constant state of hyper-alertness. This keeps your blood glucose levels high. As a result, it increases your risk of diabetes over time.
Yoga, meditation, exercise and stress management are some ways to prevent rising blood sugar from stress. You can likewise enjoy a soak in the hot tub, spa or get a massage.
7. Get Enough Sleep
Sleep is the time when your body recovers and repairs itself. Thus, it is important to get enough shut-eye. This way, your body and brain are able to restore themselves to peak condition.
On the other hand, lack of sleep or poor quality sleep negatively affect glucose tolerance. It also increases your risk of diabetes.
Sleep deprivation gets in the way of your body being able to rebuild and repair its tissues. It also disrupts your hormones, leads to weight gain and higher blood sugar.
Additionally, not getting enough sleep leaves you tired the next day. To compensate, you’ll turn to food to provide your body with extra energy. These added calories not only push your blood sugar up, they also make you gain weight.
Research also notes that poor sleep causes hormonal disruption. This can be from poor quality sleep or lack of sleep. Whatever the cause, be it your mattress, pillow or insomnia, it results in increased appetite and hunger. Both of which aggravate the situation.
Too Much Sleep is Bad As Well
 It’s worth noting that too much sleep is just as bad as not getting enough sleep. Japanese researchers discovered that sleeping between 6.5 to 7.4 hours nightly is optimal. This duration results in the lowest HbA1c (Hemoglobin A1c) levels.
It’s worth noting that too much sleep is just as bad as not getting enough sleep. Japanese researchers discovered that sleeping between 6.5 to 7.4 hours nightly is optimal. This duration results in the lowest HbA1c (Hemoglobin A1c) levels.
As you get farther away from this sweet spot, you experience a gradual increase in average blood sugar levels. Those who slept less than 4.5 hours experienced the highest levels. They were followed by those who slept 8.5 hours or more.
Here are some tips to help you sleep better.
8. Check Your Blood Sugar Levels Regularly
Whether you’re diabetic or not, checking your blood sugar regularly is an important step in staying healthy. In the past, only adults were susceptible to diabetes. As such, type 2 diabetes used to be called adult-onset diabetes.
All that has changed. Today, children as young as 9 years old are being diagnosed with the condition. This makes it more important to regularly have yourself tested.
- If you don’t have diabetes. Make sure that the standard blood sugar lab tests are included in your annual checkup. This will help you be aware of any issues before they become serious.
- If you’re pre-diabetic. You’ll need to be more vigilant. The American Diabetic Association (ADA) recommends getting checked for type 2 diabetes once every 2 years. You may also want to consult with your doctor steps you need to take to prevent your condition from becoming full-blown diabetes.
- If you have diabetes. Regular monitoring is needed. Checking your blood sugar daily is important. Common times include before each meal, two hours after eating as well as before, during and after a workout.
Regular monitoring allows you to stay on top of your health. Here is the American Diabetes Association’s Nutrition Recommendations and Interventions for Diabetes guide.
Keeping tabs on your blood sugar levels before and after meals also allows you to better understand how your body reacts to certain food.
9. Stop Smoking
 Cigarettes and cigarette smoke contain over 7,000 toxic chemicals. These include nicotine, lead, arsenic, ammonia, formaldehyde and hydrogen cyanide. What’s worse is, everyone around the smoker is affected.
Cigarettes and cigarette smoke contain over 7,000 toxic chemicals. These include nicotine, lead, arsenic, ammonia, formaldehyde and hydrogen cyanide. What’s worse is, everyone around the smoker is affected.
Besides harming your lungs, smoking also increases blood sugar. Each time you breathe in cigarette or tobacco smoke, be it as the smoker or from second-hand smoke, you experience a rise in blood glucose levels.
A study reveals that both diabetics and non-diabetics saw increases in their blood sugar levels after smoking cigarettes. Additionally, a second round of smoking resulted in an even higher increase in blood glucose.
The study did note that nicotine free cigarettes didn’t cause an increase in blood sugar levels. The same was true for smoking tobacco cigarettes without inhaling the smoke.
In some situations air purifiers for smoke works well, at least for clearing second-hand smoke from the surroundings.
How to Lower Your Blood Sugar Naturally with Diet
10. Limit Sodas, Energy Drinks, Sports Drinks and Sugary Drinks
Most store-bought drinks today are loaded with sugar. While sugar does make these drinks taste good, it also makes them a risk for metabolic disorders.
Sodas, Juices and Sugary Drinks
Sodas and juices are two of the most popular sugary drinks around. If you want to keep your blood sugar in check, it’s best to avoid them. Studies have shown that sugar-sweetened beverages are linked to higher blood sugar. They also increase your risk of type 2 diabetes and metabolic syndrome.
Those who drank 1 to 2 servings of sugary drinks daily had a 26% higher risk of developing type 2 diabetes compared to those who consumed less than 1 serving per month.
Conversely, research suggests that drinking water, tea or coffee instead of sugary drinks reduced your risk of diabetes.
Sports Drinks
 Besides sodas and juices, sports drinks also contain a lot of sugar. Sports drinks are used to replace fluids and electrolytes lost during sports or exercise. They rehydrate you and replenish your body’s electrolytes.
Besides sodas and juices, sports drinks also contain a lot of sugar. Sports drinks are used to replace fluids and electrolytes lost during sports or exercise. They rehydrate you and replenish your body’s electrolytes.
Additionally, sports drinks contain a good amount of carbohydrates. These are often in the form of sugar. Some brands also include caffeine in their beverages.
Sports drinks have been proven to be beneficial for performance and hydration. Unfortunately, research shows that most people who consume these beverages don’t need them. That’s because they aren’t active enough to require replenishment.
As a result, you’re getting more carbs and sugar than you normally would.
Energy Drinks
Energy drinks are another culprit. Energy drinks are designed to give you extra energy. This helps you power through long work hours or cram for your exam. Like sports drinks, they contain a good amount of sugar.
In addition, most energy drinks include caffeine as one of their ingredients. The caffeine and sugar contribute to increased blood glucose levels. This combination also forces your body to release more insulin to clear the glucose from your bloodstream.
With repeated use, energy drinks increase your risk of diabetes.
11. Cut Down on the Sugar
Research shows that consuming high amounts of sugar is linked to diabetes. High consumption of sucrose and fructose both increase your risk of the disease.
In fact, a 2014 study of data from 165 countries found that higher per capita consumption of sugar led to the increased occurrence of diabetes.
Added sugar in large quantities puts extra stress on your pancreas and liver. Left unchecked over time, it not only harms these organs but also damages them. Your pancreas produce insulin to process glucose from the food you eat. The more sugar you consume the harder it has to work. In the same way, large amounts of sugar negatively affect your liver, which has to metabolize it.
That said, moderate intake of sugar isn’t bad. This is according to researchers from Brigham and Women’s Hospital and Harvard Medical School. They note that moderate amounts of sugar can be part of a healthy diet.
Bottom line is, you can enjoy sugar. But, keep it in check.
The American Heart Association recommends that men consume no more than 9 teaspoons of sugar a day. That’s equal to 36 grams of sugar or 150 calories. For women, they recommend a limit of 6 teaspoons or 20 grams of sugar (100 calories) daily.
12. Control Your Portions
 Eating smaller portions during meals is one of the best ways to limit the calories you consume. It also helps you control and lose weight.
Eating smaller portions during meals is one of the best ways to limit the calories you consume. It also helps you control and lose weight.
Researchers at Pennsylvania State University note that we tend to consume more calories when given larger portions. In the study, giving subjects smaller portions resulted in lower food intake. And, better calorie restriction.
Using smaller plates, measuring your food and reading food labels are some ways you can control how much you eat. Additionally, taking your time to enjoy every bite and eating out less also help.
Ideally, your meals should consist of 50% vegetables, 25% protein, and 25% starch. Also, having 3 balanced meals daily will help limit food cravings in between.
These simple strategies will help limit the number of calories you consume. It will also help you lose weight along the way. Weight loss, as discussed earlier, helps improve blood sugar control. It also lowers your risk of diabetes.
13. Be Careful with Increasing Meal Frequency
You’ve probably heard that eating many smaller meals throughout the day is better for regulating blood sugar. In principle, it sounds logical.
But, science says otherwise.
Research suggests that fewer, bigger meals will cause your blood sugar to spike more. But, they also tend to keep your overall blood glucose level lower on average. Meanwhile, frequent meals keep your blood sugar elevated throughout the day. The latter being more dangerous in increasing your risk of type 2 diabetes.
A similar study notes that eating larger meals less frequently not only keeps glucose levels lower throughout the day, it also improved appetite control.
One common issue with frequent meals is people often don’t reduce the size of their meals. So, they end up eating more calories.
Because you need to eat many times throughout the day, you eventually fall into the habit of reaching for unhealthy snacks like chips and pastries.
Too Few Meals is Bad as Well
Conversely, eating too few meals is likewise detrimental. This is according to a study by the National Institute on Aging Intramural Research Program. Subjects who consumed only 1 large meal daily experienced increases in fasting blood sugar. They also had delayed insulin response and impaired morning glucose tolerance.
It is for this reason that many fasting protocols like intermittent fasting are only done for short periods of time. This allows you to gain their benefits without overdoing it.
14. Regulate Your Carbs
 Along with sugar, eating a lot of carbs is linked to higher blood sugar and increased risk of diabetes. Carbohydrates are broken down by your body into sugars. It then releases insulin to make these sugar usable to cells.
Along with sugar, eating a lot of carbs is linked to higher blood sugar and increased risk of diabetes. Carbohydrates are broken down by your body into sugars. It then releases insulin to make these sugar usable to cells.
The more carbs you consume, the more insulin your pancreas needs to secrete. Over time, the stress of overproduction causes it to break down. This limits the amount of insulin it can produce, leading to high blood sugar.
Counting carbs is one effective way of controlling carbohydrate intake. Additionally, low carb diets have been shown to work well in the long term.
15. Opt for Low Glycemic Index Foods
 Besides quantity, the quality of carbs is just as important.
Besides quantity, the quality of carbs is just as important.
Glycemic index (GI) and glycemic load (GL) are two popular ways of assessing the body’s glycemic response to food. A meta-analysisfound that compared to high GI diets, low GI diets resulted in lower HbA1c.
Low glycemic index foods don’t spike your postprandial blood sugar as much as high GI foods. This gives you better blood sugar control after meals. The chart on the right shows the typical post-meal glucose responses to high and low GI meals.
Australian researchers also note that a high GI diet increases your risk of type 2 diabetes by 33% compared to a low GI diet. Additionally, a high GI or GL diet that’s low in fiber pushes that risk up to 50%.
Finally, a review of 24 studies discovered that the every glycemic index point counts. For each 5 GI point increase, your risk of developing type 2 diabetes goes up by 8%.
16. Mix High GI Foods with Low GI Foods
The good news is, you don’t have to cut out high glycemic index foods totally. The key is moderation and controlling quantity. Also, mixing low GI food with high GI food brings down the total GI of your meal.
This allows you to enjoy foods like pasta, candy, cakes, cereal, and potato. The catch is that you should pair them up with low GI foods like non-starchy vegetables and protein.
A Chinese study reveals that combining high GI food like white rice and bread, with low GI options brings down the total glycemic index of the meal. The researchers used 9 different meal combinations in total.
Change in Glycemic Index of Rice After Combining Low GI Foods
In each of the situations, total GI for the meal went down significantly after adding low glycemic food to rice.
| Food | GI | % change |
| Rice only | 83.2 | n/a |
| Rice with stir-fry pork | 72.0 | -13.46% |
| Rice with stir-fry pork and celery | 57.1 | -31.37% |
| Rice with stir-fry garlic sprout | 57.9 | -30.41% |
| Rice with stir-fry garlic sprout and eggs | 62.8 | -24.52% |
Change in Glycemic Index of Bread After Combining Low GI Foods
Similar results were seen with bread. Adding fat and protein brought the GI of the meal down.
| Food | GI | % change |
| Steamed bread | 80.1 | n/a |
| Steamed bread with butter | 68.0 | -15.11% |
| Steamed bread with beef | 49.4 | -38.33% |
Their results show that adding low GI foods like protein and vegetables brings down the total glycemic index of a meal. Additionally, fats and fiber also aid in lowering post-meal blood sugar.
Varying Combinations of Carbs and Glycemic Index Matters
It’s also worth noting that varying combinations of carbs and GI affect your blood sugar and insulin levels as well. In their experiment, researchers tested 4 different diets to see their effects on glucose, insulin and hunger levels. The 4 diets were:
- HGI-HC: High GI, high carb diet
- HGI-LC: High GI, low carb diet
- LGI-HC: Low GI, high carb diet
- LGI-LC: Low GI, low carb diet

Results showed that compared to the high GI, high carb diet, the other diets produced lower levels of glucose and insulin throughout the day.
Interestingly, average blood sugar is lower from a low GI, high carb diet compared to one that’s high GI, low carb diet. But, they produce similar average insulin levels.
17. Limit Red Meat and Avoid Processed Meats
 Recent research suggests that red meat and process meats increase your risk of cancer. In addition to that, they also increase your risk of diabetes.
Recent research suggests that red meat and process meats increase your risk of cancer. In addition to that, they also increase your risk of diabetes.
A meta-analysis found that one serving of meat per day increases your risk of type 2 diabetes. The type of meat and how much you consumed also mattered.
With regards to your risk, adding one serving results in the following change in risk of diabetes.
- Unprocessed meat: +12%
- Processed meat: +32%
- Total red meat consumption: +14%
A similar study also confirmed the results. It noted that:
- 100 grams of unprocessed red meat a day: +19% risk
- 50 grams of processed red meat per day: +51% risk
As such, it may be a good idea to cut down on red meat consumption. This is especially true with processed meats, including bacon, pastrami, sausages and hot dogs.
Alternatives to Meat
Alternatively, opt for chicken, turkey, fish, and seafood. They’re leaner. And, they don’t come with the risks that red meat does.
Plus, using healthier cooking methods like baking, steaming and grilling also help. These cooking methods don’t use as much oil.
18. Enjoy Fish
Eating fish in place of meat cuts out the negative effects of red meat. It also lets you add protein to your meals, which helps lower its glycemic index.
That said, fish are a mixed bag when it comes to reducing blood sugar. Because they don’t contain carbs, they don’t elevate your glucose and insulin levels.
A few studies including one by Cambridge researchers note that consuming 1 or more servings of fish helps reduce the risk of diabetes. Shellfish, on the other hand, increases your risk.
However, a meta-analysis of 16 studies related to the matter reveals that consuming fish or seafood doesn’t harm or help diabetes risk. Additionally, Omega-3 fatty acids also didn’t offer any benefit.
19. Eat More Green Leafy Vegetables
Fruits and vegetables help regulate blood sugar thanks to their fiber content. In doing so, they cut your risk of type 2 diabetes. Interestingly, the total amount you eat isn’t related to diabetes risk.
What’s more important is how much green, leafy vegetables you consume. Eating green, leafy veggies is inversely related to developing diabetes. This is according to a 2012 study published in the European Journal of Clinical Nutrition.
A similar study notes that the fiber in vegetables, specifically yellow, cruciferous, and green, leafy ones cut diabetes risk.
20. Don’t Be Afraid of Fats
 Dietary fats have gotten a bad rap over the years. So much so that low-fat diets and products have popped up all around us.
Dietary fats have gotten a bad rap over the years. So much so that low-fat diets and products have popped up all around us.
The thing is, fats aren’t necessarily bad. With blood sugar and diabetes, fats can be a good thing.
Research reveals that the amount of fat you consume isn’t linked to your risk of diabetes. Additionally, following a low-fat diet doesn’t cut your risk either.
Fats help regulate blood sugar because they slow down the absorption of carbohydrates in your digestive tract. This prevents your glucose levels from spiking. Instead, you see a more gradual rise over a longer period of time.
The Type of Fat is Important
With dietary fat, the most important thing is choosing the right types of fat.
Research published in PLOS Medicine suggests that different types of fats have varying effects on blood sugar. Additionally, replacing carbs with fats can also help with glucose regulation.
It notes that switching out 5% of calories from carbs to saturated fat had little effect on HbA1c. But, when the same 5% of carbs was swapped out for monounsaturated fats, HbA1c fell by 0.09%. HbA1c fell by 0.11% when polyunsaturated fat was used.
Similarly, a 2001 study indicates that polyunsaturated fatty acids cut diabetes risk while trans fat increased the risk.
Bottom line: Add unsaturated fats. Keep saturated fats in check. Avoid trans fat.
21. Up Your Fiber Intake
Like fats, fiber slows the absorption of sugar. Thus, allowing for a slower, steadier rise in blood glucose after meals.
Studies reveal that consuming high fiber diets or supplementing with fiber are beneficial in controlling blood sugar. It notes that diets up to 42.5 grams of fiber or taking up to 15 grams of soluble fiber supplements daily brings down HbA1c by 0.55% and fasting blood sugar by 9.97 mg/dL.
Additionally, soluble fiber seems to be more effective for blood sugar control. A 2002 studylearned that soluble fiber helps lower HbA1c and fasting glucose in both type 1 and type 2 diabetics. It also reduced LDL and total cholesterol.
The daily recommended intake of fiber is 38 grams per day for men and 25 grams a day for women.
22. Mind Your Coffee (and Caffeine)
 Coffee, because of its caffeine content, has a strange relationship with blood sugar.
Coffee, because of its caffeine content, has a strange relationship with blood sugar.
In the short term, it increases both blood sugar and insulin levels. But, long-termcoffee drinkers experience lower risks of diabetes. Better yet, each extra cup you drink causes that risk to drop 7% lower.
Researchers in India found that those who drank 4 or more cups of coffee daily had much a lower chance of developing diabetes compared to those who drank less than 2 cups a day.
If you don’t like the negative effects of caffeine but want the benefits of coffee, go decaf. Researchsuggests that decaffeinated coffee contains many of the benefits of regular coffee. This includes its blood sugar lowering effects.
Careful with Store-Bought and Instant Coffees
One caveat is that of store-bought and instant coffees. While these products do contain similar benefits, they’re often loaded with sugar. This gives you both good and bad effects.
The same is true for some products in cafes.
23. Choose the Right Breads
Bread is loaded with carbohydrates. As such, you’ll find most of them high up on the glycemic index scale.
White bread in different forms is refined starch. This causes it to act similar to sugar once your body digests it. As such, it makes your blood sugar spike up quickly.
The good news is different types of bread have varying effects on blood glucose and insulin response. Studies show that less refined options and those high in fiber blunt these spikes.
In general, whole grain and high fiber breads are better for blood sugar control. Other types that are beneficial include sprouted breads, whole rye, and sourdough. The more fiber the bread has, the more gradual the rise in your glucose levels.
24. Not All Rice are Equal
 Like bread, rice is another meal staple that contains a large number of carbs.
Like bread, rice is another meal staple that contains a large number of carbs.
White rice, in particular, is associated with higher risk of type 2 diabetes. Researchstates that Asian populations that consumed more white rice had a higher incidence of diabetes. This was especially true when compared to western populations that consumed less white rice.
In contrast, brown rice which is whole grain helps lower diabetes risk. Researchers from Harvard’s School of Public Health found that having 2 or more servings of brown rice weekly, lowered your risk by 11%.
On the other hand, eating 5 or more servings of white rice a week resulted in a 17% increase in diabetes risk compared to having less than 1 serving a month.
They also mention that replacing 50 grams of white rice a day with brown rice cuts your risk of diabetes by 16%. Better yet, swap out the rice for whole grains to get a 36% improvement.
25. Understand Your Oats/Oatmeal
Oats and oatmeal are considered health foods for good reason. Study after study has found that it is beneficial in lowering your risk of heart disease and type 2 diabetes.
Whole grain oats have been shown to cut total cholesterol, triglycerides and LDL cholesterol as well. It also reduces fasting blood sugar, postprandial glucose, and HbA1c.
Oats are high in fiber. This helps slow the rate at which your body digests and absorbs carbs. In doing so, it helps regulate blood sugar.
The Type of Oats Matter
Not all oats are created equal. How much processing it goes through affects it glycemic index.
This is why whole oat groats are much better than instant oats for blood sugar control. Although, you probably won’t notice it just by looking at the nutrition label.
In a systematic review of whole grain processing, researchers found that instant oats and quick cooking oats resulted in the highest glycemic responses. The two foods had GIs of 75 and 71, respectively. Steel cut oats, large-flake oats and muesli & granola fared much better. They had GI levels of 55, 53 and 56, respectively.
So, if you’re looking to control blood sugar spikes, go for steel cut oat, large-flake oats or muesli & granola instead of instant or quick cooking oats. Whole oat groats are the best option. But, they also take a very long time to cook.
Finally, skip the flavored varieties because they contain a lot of added sugars and artificial flavors.
26. Go With Whole Grains
In addition to oats, try other types of whole grains as well. Many are better options than white bread and rice, which are refined starches.
Using data from previous studies, researchers note that consuming whole grains cut diabetes risk. On the other hand, white rice was linked to higher incidence of the disease. This led the team to conclude that replacing refined grains with whole grains was a good choice if you want to prevent type 2 diabetes. Further, they suggested consuming at least 2 servings of whole grains daily to achieve this.
A similar study, this time using long-term data, found that on average, those who ate more whole grains had smaller waistlines, lower BMI and weighed less than those who ate the least amount of whole grains. Also, eating whole grains resulted in lower glucose and cholesterol levels.
It’s worth noting that how well a whole grain affects glucose tolerance and insulin resistance depends on a number factors. These include:
- Their particle size and processing. The less processing, the better.
- Amount of fiber they contain. The more fiber, the better.
- Amylose and amylopectin content. The more of these starches they contain, the better.
- Its viscosity. The more viscous, the better.
Beware of Misleading Labels
One of the issues with whole grains is they’re often confusing.
The best way to know if you’re actually getting whole grain is to go straight to the ingredients on the product’s back label. Here, you’re looking for the word “whole”. Examples include “100% whole grain” and “100% whole wheat”.
Just as importantly, the “whole” ingredient should be the first on the list.
Also, avoid the following ingredients that may sound like whole grain, but aren’t.
- Multi-grain
- Contains whole grain
- Made with whole grain
- Made with whole wheat
- 100% wheat
- 7 grains
- Cracked wheat
- Bran
Try Other Types of Whole Grains
In addition to the common whole grain breads, pasta, oats and brown rice, there are a number of other good options you can try. These include:
- Quinoa
- Barley
- Bulger
- Mullet
- Buckwheat
27. Choose Your Fruits Wisely
Eating fruits is part of a healthy diet. They contain lots of nutrients including vitamins and minerals. Additionally, many fruits are high in fiber. This helps slow down the rate of carb absorption.
In a 7 year study involving 500,000 Chinese participants, eating fresh fruit daily accounted for a 12% lower risk of diabetes compared to those who didn’t eat fruits. In those who had diabetes, having fruits 3 times a week caused a 17% drop in their risk of dying. It also reduced their risk of complications from diabetes by 13% to 28%.
Fruits Vary in Sugar Content
Not all fruits are equal. This is true in terms of nutritional value as well as their sugar content. As such, fruits that contain higher amounts of sugar don’t offer as much benefit as low sugar varieties.

Harvard University researchers note that consuming 3 servings of whole fruit a week helps reduce your risk of type 2 diabetes. But, they also discovered that some fruits are more effective than others.
Blueberries offered the most benefit cutting risk by 26%. Grapes, raisins and prunes likewise produced double digit improvements. Grapefruit, bananas, apples and pears had moderate reductions.
| Fruit | Type 2 Diabetes Risk Reduction (%) |
| Blueberries | 26% |
| Grapes | 12% |
| Raisins | 12% |
| Prunes | 11% |
| Apples | 7% |
| Pears | 7% |
| Bananas | 5% |
| Grapefruit | 5% |
| Peaches | 3% |
| Plums | 3% |
| Apricots | 3% |
| Oranges | 1% |
Meanwhile, there are some fruits that can increase your risk. These included strawberries (+3%) and cantaloupes (+10%).
Ripeness
Finally, the riper the fruit, the more sugars it has. This is why ripe fruits taste better.
The ripeness of a fruit, especially starchy fruits, influences their glycemic index. This is because as the fruit ripens, its starches become less resistant.
One example is banana. Ripe bananas are softer and sweeter. They also have an average GI of around 65. Meanwhile, green bananas, are harder and less sweet. But, their GI is only around 40.
Cooking fruit basically accelerates the ripening process. As such, it also results in a higher glycemic index.
28. Stay Away from Dried Fruits or Limit Them
 While fruits are healthy and generally safe for blood sugar, there are a few types of fruits you should avoid. These are namely dried fruits, canned fruits, and fruit juices.
While fruits are healthy and generally safe for blood sugar, there are a few types of fruits you should avoid. These are namely dried fruits, canned fruits, and fruit juices.
Dried Fruits
Dried fruits are fruits that have been dehydrated. They’re tastier because their water content has been removed. This results in a higher concentration of flavor and nutrients. Unfortunately, it also makes each small bite loaded with sugar.
The USDA states the following sugar content in common dried fruits.
- Dates: 64% to 66%
- Raisins: 59%
- Apricots: 53%
- Figs: 48%
- Prunes: 38%
Thus, just eating a few of these can cause your blood sugar to spike. For this reason, it’s wise to eat only a little at a time if you want to keep your blood sugar down.
Canned Fruits
Canned fruits are convenient. They save you from having to peel or slice. But, they’re also loaded with added sugars. The sugar helps preserve them while making them taste better as well. In fact, fruits canned in syrup often contain more sugar than sodas.
If you do go for canned fruits, opt for those packed in water. Frozen fruits that don’t have added sugars are also another option.
Fruit Juices
Here, we’re talking about commercially packed juices. We’ve discussed them earlier along with sugar-sweetened beverages.
The problem with store-bought fruit juices is they contain a lot of sugar. While they still have vitamins and other nutrients, they also push your blood glucose up fast.
The best way to enjoy fruit juices it to make them at home, either with a juicer or blender. This allows you to enjoy the fruit’s benefits without the extra sugar.
Between juicing and blending, we prefer the latter. Blending fruits and vegetables keep their fiber and skin intact. Fiber helps lower blood sugar and diabetes risk, while the skin often contains the most nutrients.
29. Nuts and Peanut Butter
Nuts contain unsaturated fats, fiber, and protein. Plus, they don’t contain any sugar. This makes them a healthy choice for anyone looking to control their blood sugar.
Research involving more than 80,000 women in 11 states over a period of 16 years backs this up. The study found that consuming nuts or peanut butter 5 times a week lowered diabetes risk by 24% and 21%, respectively. Eating walnuts twice a week also helps reduce this risk by 15% compared to those who rarely ate nuts.
In addition to lowering your risk of type 2 diabetes, nuts also contain phytosterols which along with the healthy fats, help improve cholesterol.
30. Try Some Fenugreek Seeds
Fenugreek seeds aren’t as well-known as chia, flax or pumpkin. But, they work well in improving blood sugar and insulin resistance.
Studies found that these seeds help improve fasting blood sugar, post-meal blood sugar, cholesterol, and insulin response in both type 2 diabetic and pre-diabetic individuals.
Fenugreek seeds contain soluble fiber, which helps slow down sugar absorption in the body. Additionally, they’re easy to incorporate into food and drinks.
31. Enjoy Alcohol Moderately
Like coffee, alcohol increases your blood sugar in the short term and lowers it in the long term.
Alcoholic beverages contain a good amount of carbs. This causes your blood sugar to rise soon after drinking. But, several hours later, you’ll see your glucose levels drop.
More importantly, drinking moderate amounts of alcohol (1-2 glasses a day) is known to prevent your risk of diabetes.
Researchers learned that both men and women have a U-shaped diabetes risk response to alcohol.

- The optimal amount for men is 22 grams of alcohol daily. This offered a 13% less chance of developing diabetes compared to those who didn’t drink. The protective effect stayed on until around60 grams/day.
- For women, the optimum amount of alcohol was 24 grams a day. Here, they experienced a 40% lower risk of diabetes compared to non-drinkers. The protective effects were sustained under 50 grams a day.
32. Have Some Dairy
While it may sound ironic, full-fat dairy is good for your blood sugar. Contrary to popular belief, it also helps you lose weight.
Eleven of 16 studies found that high-fat dairy helps lower the rate of obesity. Meanwhile, the same isn’t true for low-fat dairy. This is according to a report published in the European Journal of Nutrition.
Another study notes that people who consumed the most full-fat dairy had a 62% less chance of developing type 2 diabetes. These individuals also had lower amounts of abdominal fat, triglycerides and inflammation.
Their finding is backed up by a few other studies. However, it is worth noting that there are also some studies that show no link between dairy and diabetes.
33. Better Yet, Have Yogurt
 Yogurt is produced from milk by fermenting it. What makes it stand out is the presence of probiotics. These are healthy bacteria that improve digestion.
Yogurt is produced from milk by fermenting it. What makes it stand out is the presence of probiotics. These are healthy bacteria that improve digestion.
A study published in Evidence Based Care Journals notes that consuming probiotics from yogurt helps lower blood sugar and HbA1c in type 2 diabetics. Additionally, it improves blood pressure.
Yogurt, especially Greek yogurt, is a healthier option to milk or ice cream. This is especially true if you want to gain the benefits of healthy probiotics.
Avoid Fruit-Flavored Yogurt
With yogurt, we recommend sticking with the plain versions with no sugar added.
Most yogurts found on store shelves are flavored. These are loaded with added sugars and carbs. As such, they add extra calories. And, also negatively affect your blood sugar levels.
34. Go Vegetarian or Vegan a Few Days a Week
Studies suggest that consuming a vegetarian diet cuts your risk of diabetes by nearly 30%. In addition, it is a good way of keeping your average blood sugar in check. A systematic review and meta-analysis observed that going vegetarian can lower your HbA1c by nearly 40%.
Plant vs. Animal Source of Protein
Using data from past trials, Canadian researchers reveal that replacing animal protein with plant sources improves blood sugar control. Doing so reduced HbA1c, fasting blood sugar and fasting insulin by averages of 15%, 53%, and 10%, respectively.
A vegetarian or vegan diet relies on non-animal sources of protein. This cuts down the amount of fat you eat. In doing so, it decreases the saturated fat you consume. This helps lower your risk of heart disease, insulin resistance and some cancers.
Additionally, plant sources of protein don’t contain cholesterol. Plus, they are often good sources of phytonutrients and fiber.
Studies also note that plant-based diets help you lose weight, decrease saturated fat and improve your gut microbiome.
35. Be Careful with Granola, Snack Bars, Protein Bars and Nutrition Bars
High protein, high fiber snack bars are beneficial for anyone looking to regulate their blood sugar. They are a convenient way of adding healthy calories. Research also indicates that replacing refined carbs with fiber and protein improves your glucose and insulin profiles.
Many Snack Bars are Unhealthy
That said, most of the snack bars found in stores are loaded with sugars, fat, and artificial flavoring. For this reason, it’s important to read the ingredients when you’re buying a protein, granola or other types of snack bars.
Ideally, you want something that has a good amount of protein, fiber, and healthy fats. On the other hand, avoid those high in carbs and sugar of any form. This includes artificial sweeteners, high fructose corn syrup, and table sugar.
How to Lower Your Post Meal Blood Sugar Fast
36. Walk After Meals
 One of the simplest ways to blunt the effect of post-meal blood glucose spikes is to take a walk after you’ve eaten.
One of the simplest ways to blunt the effect of post-meal blood glucose spikes is to take a walk after you’ve eaten.
A report published in Diabetes Care notes that walking 15 minutes after each meal helped improve 24-hour glycemic control in elderly individuals at risk of glucose intolerance. It was also more effective than 45 minutes of continuous walking done once a day.
This concept works just as well in young, healthy individuals and those with diabetes. An earlier report in the same publication found that being inactive resulted in a 113% higher blood sugar level compared to being active post meal. In subjects with diabetes, the increase was 145% higher in those who were inactive.
Subjects saw a 30 mg/dl improvement in their glucose levels with physical activity. The effects began 10 minutes after they started walking and lasted up to 5 minutes after they stopped.
Pre-Meal vs. Post Meal Walking for Lower Blood Sugar
Interestingly, the time you exercise affects the end result. A study shows that walking 20 minutes at a comfortable pace after meals lowers blood glucose levels more than when it’s done before eating.
Timing is Key
 Research also shows that starting exercise 30 minutes after your meal and continuing it for 30 to 60 minutes works well. This allows the body to work off the incoming glucose molecules from the food you just consumed.
Research also shows that starting exercise 30 minutes after your meal and continuing it for 30 to 60 minutes works well. This allows the body to work off the incoming glucose molecules from the food you just consumed.
In doing so, you burn off the extra sugar before it is allowed to accumulate and peak. This can be seen in the chart on the right which depicts the post-meal blood sugar curves of normal and diabetic individuals.
From the chart, you’ll see that there’s a timing differences between diabetics and non-diabetics. This is due to the impaired glucose metabolism caused by diabetes. As a result, if you have diabetes, exercising 1 or 2 hours after eating is optimal.
Results from the Big Blue Test shows that 30 minutes of physical activity done at 1 or 2 hours post meal yielded drops of 49.3 mg/dL and 46.4 mg/dL, respectively. Meanwhile, exercise started 30 minutes after eating lowered blood glucose by 34.3 mg/dL. And, doing it after 3 hours or more post-meal resulted in a 19.6 mg/dL decrease.
37. Always Eat Protein with Your Carbs
For the most part, carbs are responsible for increasing blood sugar post meals. On the other hand, studies show that protein doesn’t. This is true for both diabetics and non-diabetics.
Adding protein to any meal that contains carbohydrates effectively lowers the glycemic index of the combined meal. As such, increasing dietary protein leads to lower postprandial blood glucose levels. It also improves overall blood sugar control.
Protein Can Also Increase Blood Sugar
It’s worth noting that protein may also be broken down by your body into glucose. This process is called gluconeogenesis. Often, this happens when you cut down on carbs. In response, your body uses a less efficient source of fuel, protein, to produce energy.
In the same way overeating protein can also result in blood sugar increases. Although you’ll see this elevation happen several hours after the meal.
38. Eat Your Veggies and Protein First
This is a sneaky trick you can use to help reduce the blood sugar spikes after eating. Instead of eating all your food at the same time, try splitting them up.
Eating vegetables, protein, and fats before carbs decreases blood sugar spikes after meals.
A study published in the Journal of Biochemistry and Nutrition shows that the order you consume your food affects blood glucose excursions.
Here, subjects were instructed to eat their vegetables for 5 minutes. Then, followed by the main dish for another 5 minutes. Finally, they left the bread or rice for the last 5 minutes.
The image below shows the mean blood glucose levels of the subjects in a 24 hour period.
- The dotted lines represent the subjects with normal glucose tolerance. The full lines show those with type 2 diabetes.
- Meanwhile, the red lines note the blood sugar levels in meals where the subjects ate carbs before vegetables. The green lines the opposite order.
 In both diabetics and non-diabetics, food order affects blood sugar, In both cases, glucose was lower when you eat vegetables and protein before carbohydrates.
In both diabetics and non-diabetics, food order affects blood sugar, In both cases, glucose was lower when you eat vegetables and protein before carbohydrates.
Extending the Time to 15 Minutes
Increasing the time between eating your vegetables and protein from carbs improves the results.
Researchers discovered that eating carbohydrates 15 minutes after vegetables, protein, and fats improves the results of the study above.
Blood Sugar When Eating Carbs First or Last (in mg/dL)
| Time (min) | Eat Carbs First | Eat Carbs Last | Change (%) |
| 0 | 106.7 | 107.3 | 0.5 |
| 30 | 156.8 | 112.0 | −28.6 |
| 60 | 199.4 | 125.6 | −37.0 |
| 120 | 169.2 | 140.8 | −16.8 |
Compared to eating carbohydrates first, leaving them last resulted in post-meal blood glucose decreases of 29%, 37% and 17% at 30, 60 and 120 minutes after the start of the meal, respectively.
39. Include Healthy Fats with Each Meal
Besides protein, only fats are able to negate the blood sugar effects of a high carbohydrate meal. Thus, adding them to your meal helps reduce the effects of food on your blood sugar.
Adding Extra Virgin Olive Oil to meals helps lower 2-hour post meal blood glucose levels. In addition, it improves insulin and LDL cholesterol levels. This is according to research published in Nutrition & Diabetes.
Of course, you can use other types of fats as well. The research did a second study comparing corn oil to EVOO. While corn oil did help lower the blood sugar spike after meals, it didn’t perform as well as olive oil. Additionally, most other fats, including butter, lard, and vegetable oils, have the opposite health effects of olive oil.
40. Add a Splash of Vinegar with Your Meals
 Like fats, vinegar helps keep food in your stomach longer. It does so by partially blocking the digestion of starch. As a result, it helps reduce the post-meal blood sugar rises.
Like fats, vinegar helps keep food in your stomach longer. It does so by partially blocking the digestion of starch. As a result, it helps reduce the post-meal blood sugar rises.
Swedish researchers found that adding vinegar to white bread significantly lowers post-meal blood sugar increases. They also learned that the higher the acetic acid concentration, the larger the decrease in blood glucose rise.
Olive oil and vinegar are two staples of the Mediterranean diet. Many cultures in that region use a vinaigrette made from extra virgin olive oil and vinegar. Often, to dip their bread in before or during meals. The mixture is also used for salad dressing.
Using Vinegar and Olive Oil in Combination
Our own experiments show that both olive oil and vinegar independently blunt the rise of blood sugar after eating. But, combining 1 tablespoon of olive oil and 1 tablespoon of vinegar with your meals magnifies their effects.
41. Enjoy Some Apple Cider Vinegar
While we’re on the topic of vinegar, there’s one type that’s been shown to be very healthy, apple cider vinegar.
- Apple cider vinegar is made from crushed apples. These are fermented into alcohol. Then, turned into vinegar.
- White vinegar, on the other hand, is distilled from grains. They use a similar process to yield acetic acid.
Because of the source of their raw materials, the two have different color, texture, odor, and taste. White vinegar is healthy and has many uses. But, apple cider vinegar is notable for even more health benefits.
Like white vinegar, apple cider vinegar slows gastric emptying. In doing so, it helps slow down the rate at which carbs are turned into glucose by the body. This blunts the increase in blood sugar after eating.
Apple cider vinegar improves post-meal blood glucose. It also helps lower morning fasting blood sugar levels and improves insulin sensitivity.
42. Sprinkle Some Cinnamon on Food
 Sprinkling cinnamon on your coffee or oatmeal is one way you can reduce blood sugar spikes after breakfast.
Sprinkling cinnamon on your coffee or oatmeal is one way you can reduce blood sugar spikes after breakfast.
Research reveals that cinnamon can lower blood glucose anywhere from 10% to nearly 30%. It also improves HbA1c in type 2 diabetic patients by 10%. Cinnamon does this by slowing down the rate carbohydrates are broken down in your digestive tract. This helps curb the rise in blood sugar after eating.
Besides blood sugar, studies also show its ability to improve triglycerides, LDL and HDL cholesterol.
Adding anywhere from half a teaspoon to 2 teaspoons a day is a quick and easy way to help you regulate your blood sugar.
A Word of Caution on Cinnamon
Cinnamon offers many health benefits. But, it comes with a safety warning. The issue here isn’t with cinnamon itself. But, the type of cinnamon.
Like other spices, cinnamon comes in many varieties. The four main types are Cassia, Saigon, Ceylon and Korintje cinnamon. These variations differ in appearance, aroma, color, and taste.
Due to their similarities, Cassia, Saigon and Korintje are often classified under Cassia cinnamon. Cassia is the most common type of cinnamon found in grocery stores and supermarkets. They’re more available and very affordable.
Coumarin Content in Cinnamon
Unfortunately, they also contain high concentrations of coumarin. Coumarin is a naturally occurring flavoring substance. It is toxic to the liver in people who are sensitive to it. And, at high amounts can cause damage to the organ.
Ceylon cinnamon, also known as true cinnamon, contains much less coumarin. This makes it the best option to use. Unfortunately, it’s also very expensive. As such, you won’t see it used in many retail establishments or sold at your local grocery store.
Here’s a summary of the different types of cinnamon and their coumarin content.
| Type of Cinnamon | Coumarin Content |
| Ceylon Cinnamon, True Cinnamon, Mexican Cinnamon | 0.017 g/kg |
| Indonesian Cinnamon, Korintje Cinnamon, Padang Cassia | 2.15 g/kg |
| Saigon cinnamon, Vietnamese Cassia, Vietnamese Cinnamon | 6.97 g/kg |
| Cassia Cinnamon or Chinese Cinnamon | 0.31 g/kg |
If you don’t consume cinnamon on a regular basis, this won’t be much of an issue. But, if you enjoy it regularly, we recommend cutting down or going with Ceylon cinnamon.
43. Include Fiber with Each Meal
Increasing the amount of fiber in your diet helps your body regulate blood sugar better over the long term. Also, having fiber with every meal offers a more immediate benefit.
Eating foods high in fiber helps slow digestion. It delays gastric emptying. And, reduces post-meal glucose and triglyceride excursions. The studies, here and here, show the different effects of various types of fiber in reducing postprandial blood glucose levels.
Dietary Fiber’s Effect on High and Low GI Meals
 Adding fiber to your meals can help negate the effects of a high glycemic index meal. A studyfeatured in the Journal of Nutrition notes that a high GI, low fiber meal causes the highest increase in postprandial blood glucose.
Adding fiber to your meals can help negate the effects of a high glycemic index meal. A studyfeatured in the Journal of Nutrition notes that a high GI, low fiber meal causes the highest increase in postprandial blood glucose.
Conversely, its opposite, a low GI, high fiber meal, produced the best metabolic response.
The chart A on the right shows the blood glucose AUC (area under the curve) after eating up to 3 hours post meal.
- HG-HF represents the High GI, High Fiber meal’s results.
- HG-LF is that of the High GI, Low Fiber meal.
- LG-HF is for the Low GI, High Fiber meal.
- LG-LF is for the Low GI, Low Fiber meal.
Meanwhile, the chart B below it illustrates the insulin AUC.
The graphs show that post-meal blood sugar effects of a high GI meal can be attenuated by going high fiber. This helps reduce the post-meal blood sugar surge. In the same way, you can compensate for a low fiber meal by consuming one that has a low glycemic index.
But, as seen on the insulin AUC chart to on the right side, both these scenarios do cause larger blood insulin levels after eating compared to the low GI, high fiber meal.
44. Take Advantage of the Second Meal Effect
This is something few people are aware of. But, knowing the benefits of the “Second Meal Effect” can help you control blood sugar after meals.
Also known as the “Subsequent Meal Effect”, the second meal effect is a phenomenon where a low glycemic index meal is able to help blunt the blood sugar rise of the next meal.
As such, it helps reduce your current meal’s postprandial levels. And, positively affects the upcoming meal as well.
The chart below shows the same second meal having a lower blood sugar effect thanks to the previous meal’s low GI.
 This allows you to plan your meals in advance. In doing so, you can “splurge” on certain meals.
This allows you to plan your meals in advance. In doing so, you can “splurge” on certain meals.
For example, if you want to eat a high carb dinner, consuming a low GI lunch will help reduce your blood sugar spike tonight.
Better yet, the second meal effect works for snacks and overnight meals as well. Eating a low GI snack improves post-dinner blood sugar levels. Meanwhile, eating a low GI dinner is also beneficial to your post-breakfast blood glucose levels.
45. Freeze, Defrost, and Toast Bread
Bread is a staple in many meals. It is also one of the biggest culprits that cause blood sugar to rise after eating. If you look at its carbohydrate content as well as its glycemic index and load, you’ll notice why.
We mentioned earlier that one way to limit the post-meal glucose surge from bread is to choose the right type of bread. Also, picking one with high fiber or made with sprouted grains helps even further.
A cool trick we like to use is to freeze, defrost and toast bread.
Yes, doing so cuts down its glycemic index. In the process, it reduces the spike in blood sugar that’s often associated with it.
A 2008 study in the European Journal of Clinical Nutrition notes that freezing, defrosting and toasting homemade and commercial breads significantly reduced post-meal blood glucose and the incremental area under the glucose response curve (IAUC).

Homemade Bread
| How It’s Eaten | IAUC (in mmol) | IAUC % change |
| Fresh | 259 | 0% |
| Frozen and Defrosted | 179 | -30% |
| Toasted | 193 | -25% |
| Frozen, Defrosted then Toasted | 157 | -39% |
Commercial White Bread
| How It’s Eaten | IAUC (in mmol) | IAUC % change |
| Fresh | 253 | 0% |
| Frozen and Defrosted | 217 | -14% |
| Toasted | 183 | -28% |
| Frozen, Defrosted then Toasted | 187 | -26% |
46. With Carbs Like Rice, Pasta and Potatoes, Don’t Overcook. Cool and Reheat Them Instead
Cooking affects the glycemic index of starchy food. The longer you cook them the higher the GI becomes. This is true for pasta, potatoes and other high carb foods.
Cooking starchy food longer makes them softer. In the process, they also lose their form. When this happens, they become easier to break down during digestion. Thus, making them give up their glucose easily.
As a result, you experience a more rapid rise in blood sugar.
For example,
- Cooking pasta for 5 to 6 minutes makes it al dente. This results in a low to medium glycemic index.
- Cooking pasta for 15 to 20 minutes increases starch gelatinization. This results in a medium to high GI.
- Meanwhile, letting pasta boil for 40 minutes leaves you with a high GI.
Cook, Cool and Reheat Instead
One workaround you can do to lower the glycemic response of high carb foods is to cook it, let it cool, then reheat it.
Research found that cooling cooked rice for 10 hours at room temperature increases its resistant starch. Further, allowing cooked rice to cool at 4°C for 24 hours then reheating it produced even higher levels of resistant starch.
Separate experiments for pasta and potatoes also yielded similar results. Cooling then reheating them resulted in lower glycemic indices. Though it’s worth noting that different varieties of potatoes have varying resulting GIs.
Resistant starch is a type of starch present in carbohydrates. Much like soluble fiber, the body can’t digest it. Research reveals that resistant starch helps keep blood sugar down after meals. Additionally, it improves insulin sensitivity.
One other study also indicates that resistant starch has a “second meal effect”. Thus, it helps bring down the glycemic response of your next meal.
47. Eat Peanuts with Your Meals
 Eating peanuts with a high glycemic meal helps reduce post-meal blood sugar spikes. This is according to a study by Arizona State University’s Department of Nutrition.
Eating peanuts with a high glycemic meal helps reduce post-meal blood sugar spikes. This is according to a study by Arizona State University’s Department of Nutrition.
It found that adding vinegar or peanuts to a high glycemic load meal reduced 1-hour glucose by 55%. It also helped cut calorie consumption for the rest of the day by 200 to 275 calories.
Peanuts are easy to include in any meal. They don’t need any preparation. And, they taste good.
Unless you’re allergic to nuts, having them as an appetizer or for dessert is a quick and easy way to blunt blood sugar spikes after a high carb meal.
48. Enjoy a Drink Before Meals
Moderate alcohol consumption improves glucose response. Specifically, enjoying a drink before a meal helps reduce postprandial blood sugar by 16 to 37%.
Interestingly, beer, white wine and gin have varying effects. This is according to a study that combined each of the drinks with white bread. In the test cases, all 3 alcoholic beverages reduced post-meal blood sugar and insulin more than eating bread alone or eating bread with water.
49. Sip Some Green Tea
 Tea has many health benefits. Among them is its ability to lower blood sugar.
Tea has many health benefits. Among them is its ability to lower blood sugar.
Studies reveal that consuming 3 or more cups of tea daily lowers your risk of type 2 diabetes by 16%.
Green, black and oolong tea improve insulin sensitivity by 15 times. This is according to research by the U.S. Department of Agriculture. On the other hand, herbal teas don’t provide the same benefit.
What you add to tea matters as well.
Lemon didn’t affect its insulin benefits. But, adding 5 grams of 2% milk reduced this by 33%. Further, 50 grams of milk per cup almost negated (-90%) this positive effect.
Adding soy milk and non-dairy creamers are likewise no-no’s.
So, instead of drinking soda or sugar-sweetened fruit juices with meals, try tea. Doing so helps you cut down on calories, carbs, and added sugars. Additionally, their polyphenol content aid in fighting oxidative stress and inflammation. Both of which are major factors in chronic illness like heart disease and type 2 diabetes.
Vitamins, Minerals, Herbs, and Supplements That Help Lower Blood Sugar
50. Chromium
Some studies show that chromium supplementation helps with blood sugar control. But, its beneficial effects seem limited to diabetic individuals.
One study notes that 4 month chromium supplementation reduced HbA1c, fasting blood and 2-hour blood glucose. Additionally, it also improved fasting and 2-hour insulin levels. As a bonus, participants saw their cholesterol drop as well.
Chinese researchers observed similar results in after a 10-month follow-up. Additionally, participants said they experienced fewer symptoms from diabetes. These include reduced fatigue, thirst and urination frequency.
However, research findings are mixed.
A review of past studies notes that while chromium improves glucose and insulin metabolism, it wasn’t effective in some trials. The authors suggest that the low dose (250 micrograms or less daily) used in these trials may be one reason. They also believe that combining diabetic and non-diabetic participants was a factor.
51. Magnesium
Much like chromium, magnesium deficiency is linked to higher risk of diabetes. Conversely, having high levels of magnesium cuts your risk of the disease. This is according to a 20 year follow up study. Participants with high levels of magnesium had nearly a 50% less chance of developing diabetes compared to low magnesium individuals.
The National Institutes of Health recommends men ages 14 and above get between 400 to 420 mg of magnesium daily. Adult women need 310 to 320 mg per day.
To get more magnesium in your diet, enjoy some nuts. Almonds, peanuts and cashews are good sources. Dark, green leafy vegetables, beans, avocado whole grains, dark chocolate, and fish are other food that contain the mineral.
52. Berberine
Berberine is a supplement that’s made from a combination of herbs. It is anti-diabetic. And, studies have shown it to be beneficial for metabolic conditions, aging, inflammation and heart health.
One such research compared taking Berberine to popular diabetes drug Metformin. It found that taking 500 mg of Berberine 2 to 3 times daily for 3 months had similar blood sugar and lipid controlling effects as Metformin.
Other studies note Berberine’s ability to lower blood sugar and increase the breakdown of carbohydrates.
While effective, it does have some side effects. These include abdominal pain, flatulence, diarrhea, and constipation.
53. Vitamin D May Help
Some evidence suggests that vitamin D is inversely associated with diabetes. But, there’s more evidence for type 2 diabetes and less for type 1 diabetes.
Studies show that low levels of circulating 25-hydroxyvitamin D are linked to increased risk of type 2 diabetes. The study used data from 21 past trials involving over 76,000 participants in total. It found that every 10 nmol/L increase in 25-hydroxyvitamin D cuts diabetes risk by 4%.
Health professionals also believe that vitamin D helps with insulin sensitivity. By aiding in your pancreas’ insulin production, it is able to lower your risk of insulin resistance and diabetes.
Types of Diets for Blood Sugar Control and Reduction

In this section, we highlight the types of diets that have been scientifically proven to reduce blood sugar and improve insulin sensitivity.
For many, following specific diets is easier than remembering individual foods. It also eliminates the risk of negating these foods’ positive effects by consuming foods that you should avoid.
With complete diets, you’re better able to get a full picture of what to eat and avoid.
Instead of having to remember a long list of foods you can eat or should avoid, you have a basic framework of what to follow.
54. Mediterranean Diet
The Mediterranean Diet is one of the healthiest diets around. It emphasizes on eating fruits, vegetables, nuts, beans and whole grain.
The diet primarily uses olive oil as its source of fat. Also, it limits meat consumption. Instead, it focuses on fish and poultry as its main sources of protein.
Many studies link the Mediterranean diet to lower risk of type 2 diabetes. One such example is a 4-year study in Europe. Here, participants who followed the diet without calorie restriction had 40% lower risk of diabetes compared to those on a low-fat diet.
55. DASH Diet
The DASH Diet, or Dietary Approaches to Stop Hypertension, was created by the US National Institutes of Health. It is a dietary pattern guideline that’s aimed at reducing blood pressure.
The DASH diet does so by limiting the amount of sodium you consume. This includes added salt to meals.
It also encourages eating more fruits, vegetables, and whole gain while limiting foods high in saturated fat. Instead, it promotes lean protein and low-fat dairy.
Besides lowering blood pressure and heart disease risk, research indicates that the DASH diet also reduces your risk of diabetes.
One study reveals that following a DASH pattern of eating that’s rich in fruits, vegetables, and low-fat dairy helps lower the incidence of type 2 diabetes.
56. Vegetarian and Vegan Diets
Earlier, we mentioned that going vegetarian or vegan can help reduce blood sugar. Here, we go into the diet itself. More specifically, how different types of vegetarian diets fare with non-vegetarian diets.
A study involving over 40,000 participants observed that being vegan or vegetarian reduces the risk of type 2 diabetes compared to a non-vegetarian diet. The study also noted that all types of vegetarians, be it vegans, lacto ovo vegetarians, pesco vegetarians or semi-vegetarians fared better than non-vegetarians.
Interestingly, different types of vegetarian diets produced varying effects. The most prominent ones being BMI and risk of type 2 diabetes.
Risk of Different Types of Vegetarian Diets Compared to Non-vegetarians
| Type of Vegetarian | Risk of Diabetes | BMI |
| Vegan | -49% | -18% |
| Lacto-ovo vegetarian | -46% | -11% |
| Pesco-vegetarian | -30% | -9% |
| Semi-vegetarian | -24% | -5% |
The results indicate that animal protein is inversely associated with diabetes risk and BMI.
57. Paleo Diet
The Paleo diet is short for Paleolithic diet. It follows a dietary pattern that’s like our hunter-gatherer ancestors.
The diet promotes eating lean meat and fish along with fruits and vegetables. It also avoids grains, dairy, and refined sugar.
Research shows that following this eating pattern produces significant improvements in glucose control.
One study also suggests that it works better than the diet recommended by the American Diabetic Association. Here, those who followed the Paleo diet saw better improvements in blood sugar, lipid profiles, and insulin sensitivity.
58. Low Carb Diets
Low carbohydrate diets make logical sense considering that carbs are converted into glucose.
Compared to a high carb diet, following one that’s low in carbs reduces HbA1c and fasting blood sugar levels.
According to Australian researchers, participants who followed low carb diets over 1 year experienced larger reductions in weight, blood pressure, HbA1c, fasting blood sugar and LDL cholesterol.
A similar study notes that lowering the number of carbs also reduces belly fat, improves body composition and glucose metabolism. The latter was seen through decreases in fasting glucose and insulin. It also resulted in improved insulin sensitivity.
59. Alternate Healthy Eating Index
The Alternate Healthy Eating Index (AHEI) isn’t a diet. It is a dietary pattern that’s based on the USDA’s 1995 Healthy Eating Index (HEI).
The AHEI was created by Harvard researchers who found that the HEI didn’t improve your risk of chronic disease and death. So, they set out to create a better one. This led to the AHEI.
The AHEI is a set of dietary guidelines that involves increasing the amount of fruits, vegetables, whole grains and nuts you eat. It also encourages omega-3 fats, polyunsaturated fats, and legumes.
At the same time, it promotes lower intake of red and processed meats, trans fat, sodium and sugar-sweetened beverages.
Research suggests that following a diet that’s high on the AHEI scale improves your risk of cardiovascular disease, type 2 diabetes, cancer, and death.
This was confirmed by another study which showed that people of all ethnicities benefit from following a high AHEI diet.
60. Prudent Pattern Diet
Like the Alternate Healthy Eating Index, the Prudent diet isn’t a diet. It is a dietary pattern that includes higher amounts of vegetables, fruits, and whole grains. It is also lower in refined grains, red meats, and sugar-sweetened beverages.
The Prudent diet has many similarities with the Mediterranean and DASH diets. In addition, it has some features that are like those of the Okinawa diet, which is associated with long life.
Research shows that following a Prudent diet reduces your risk of insulin resistance by nearly 50%. Because of this, it help prevent type 2 diabetes.
Another study came to a similar conclusion when it compared the Prudent diet to the traditional western diet.
The latter study also notes that a Prudent diet offers better results on average.
It discovered that the diabetes risk difference between the highest and lowest categories of Prudent diet followers was only 15%. Meanwhile, the difference between high and low categories of western diets was 41%.
Source: https://healthgrinder.com
Disclaimer: We at Prepare for Change (PFC) bring you information that is not offered by the mainstream news, and therefore may seem controversial. The opinions, views, statements, and/or information we present are not necessarily promoted, endorsed, espoused, or agreed to by Prepare for Change, its leadership Council, members, those who work with PFC, or those who read its content. However, they are hopefully provocative. Please use discernment! Use logical thinking, your own intuition and your own connection with Source, Spirit and Natural Laws to help you determine what is true and what is not. By sharing information and seeding dialogue, it is our goal to raise consciousness and awareness of higher truths to free us from enslavement of the matrix in this material realm.
 EN
EN FR
FR

 Walking: 48.5%
Walking: 48.5%









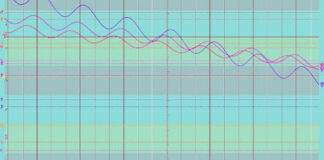










Here are more tips to help manage cholesterol! https://www.qunol.com/blogs/blog/what-you-need-to-know-about-cholesterol-management/?utm_source=respond&utm_medium=blog&utm_campaign=cholest-manage
Very informative
Best article on this topic I’ve read online so far. Thank you
Very good
Good job.
Hello,
I’m writing a book on home remedies and healthy eating. This article is a true inspiration in healing of the body.
Thank you so much for sharing.
God bless!
Thank you , lots of helpful info for pre diabetic person to follow
Good article.
Thankyou, a very long read but now I want to print it off for every diabetic I know
Excelente, Gracias